Most independent practices didn’t launch remote care programs so they could track timers, chase scattered documentation, or argue with spreadsheets at the end of every month. They adopted RPM and CCM because they believed these programs would keep patients out of the hospital, create stability in a turbulent reimbursement environment, and help them deliver more modern, continuous primary care. Yet inside almost every in-house RPM or CCM workflow, there is a moment that rarely gets acknowledged out loud. It happens when a nurse looks at the log and sees the number that makes their stomach drop: 18 minutes .
Related FairPath Resources
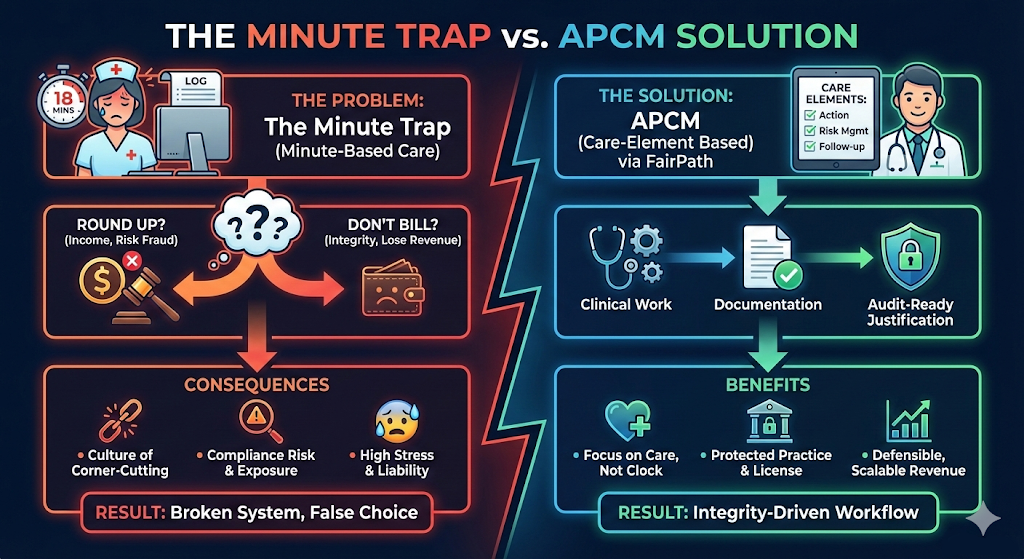
In that moment, the nurse faces a choice that should never exist in a legitimate care-management model. Do they round the time up so the practice can bill? Or do they leave it as-is and lose revenue for work that genuinely occurred? This is the moment where the system forces good clinicians into untenable decisions. This is the moment I call
the Minute Trap
.
The Minute Trap: When Good Work Collides With Bad Rules
In nearly every practice I’ve supported, the pattern is identical. The clinical work is real. The touchpoints are real. The patient benefited from the engagement. But the documentation sits just shy of the threshold, and the nurse is juggling a high patient load in an understaffed environment, often at the end of a month that’s already stretched them thin. In that moment, the nurse is not thinking like a fraudster—far from it. They’re thinking like someone who wants to do right by patients, support the physician, and avoid being the reason the practice misses out on earned revenue.
Rounding up feels like a harmless adjustment. But CMS and the OIG don’t see nuance in these situations. They see a claim that doesn’t align with the rules as written. Over time, this quiet monthly pressure reshapes culture. Teams begin to normalize comments like, “Everyone does it,” or “We’ll fix the workflow later,” or “We can’t afford to leave money on the table.” This isn’t a training issue or a sign of a disengaged staff. It’s not about hustle or work ethic. It is the predictable fallout of a structural flaw in how minute-based remote care has been designed.
Why In-House RPM Isn’t Automatically Safer
Many practices brought RPM in-house believing it would increase control, strengthen clinical alignment, and reduce expenses tied to outside vendors. And on paper, that logic seems sound. But in practice, in-house programs often carry more risk precisely because the pressure, documentation, and billing decisions all occur inside the same walls.
What I see consistently is that minutes are scattered across multiple systems, handwritten notes, or EHR messages that don’t map cleanly to billable documentation. There is rarely a single, audit-ready source of truth. Documentation and billing often drift apart, especially during end-of-month catch-up periods. And nurses—who entered healthcare to care for people, not to play timekeeper—end up responsible for both clinical continuity and revenue capture. Under these conditions, the “18-minute decision” isn’t an outlier. It’s built into the operating system of the program. The real cost of an in-house RPM program is not the staff time required to run it; it’s the compliance exposure created when documentation and billing logic don’t match.
APCM: Moving From Minutes to Care Elements
Advanced Primary Care Management (APCM) provides a way out of this cycle. Instead of tying reimbursement to a stopwatch, APCM organizes care around care elements —the actual clinical actions and interventions that define good longitudinal care. These include risk stratification, medication reconciliation, chronic condition follow-up, patient education, coordinated interventions, escalations, and longitudinal care patterns. In other words, APCM aligns reimbursement with how clinicians naturally think and work.
This framework allows practices to dramatically reduce reliance on manual minute tracking. It strengthens documentation integrity and lowers false-claim exposure. It gives physicians confidence that their license is protected. And it gives nurses permission to focus on clinical care instead of managing a countdown timer. The question for practices becomes less about whether they are “working hard enough” and more about whether their care-management structure is defensible, repeatable, and aligned with where CMS is taking primary care.
Why This Matters for 2025
CMS is steadily shifting away from minute-threshold logic and toward models that value comprehensive, longitudinal care. That shift will place increasing scrutiny on documentation quality, consistency between systems, audit readiness, and clinical justification. Practices that continue relying on hourglass-based workflows will find the pressure intensifying. Practices that embrace a care-element approach will not only reduce exposure—they’ll build a stronger foundation for growth.
Administrators, office managers, and medical directors feel this dynamic more than anyone. They are the ones balancing compliance, operations, staffing, documentation, and revenue integrity every single month. They see the 18-minute problem long before anyone puts a name to it. And the truth is: this problem is solvable. But it requires a system designed for how real care happens—not how time is captured.
A Better Next Step
If this resonates with you...if you recognize the Minute Trap in your own program…the most productive next step is simply to understand what a compliance-first, APCM-ready care-management environment actually looks like. That’s the foundation of FairPath .
FairPath isn’t built around minute thresholds. It’s built around compliance, care elements, documentation integrity, and workflows that protect the practice rather than expose it. It supports RPM, CCM, RTM, and APCM in one unified structure and eliminates the operational and ethical tension clinicians face at the end of every month.
If you want to see how modern practices are removing the Minute Trap entirely, visit:
FairPath.ai
It outlines how compliance-first design works, how APCM-style care is structured, and how practices are preparing for 2025 and beyond. Most teams don’t need to “work harder.” They need a system that reflects the reality of care, and it shouldn’t be a “minute hand”.