Chronic pain isn’t just a condition, it’s a thief. It steals time, joy, and freedom from over 51 million Americans, according to the CDC, costing the economy $560 billion a year. As someone passionate about healthcare innovation, I’ve seen how this silent struggle affects patients, families, and providers. But there’s hope on the horizon. Technologies such as Remote Patient Monitoring (RPM), Remote Therapeutic Monitoring (RTM), and Chronic Care Management (CCM) are reshaping how we manage chronic pain. Let’s explore what these tools are, why they matter, and how they’re giving people their lives back, all in a way that’s clear and deeply human.
Related FairPath Resources
The Reality of Chronic Pain
Chronic pain is pain that lingers for more than 12 weeks, often outlasting its original cause, think arthritis, fibromyalgia, or nerve damage from an old injury. It’s not just physical. It can make you miss work, skip family dinners, or feel isolated, with anxiety or depression often tagging along. The CDC says 20.6% of U.S. adults live with it, and for many, traditional treatments such as painkillers or physical therapy aren’t enough. Long drives to clinics or gaps in care can make things worse. This is where advanced solutions deliver smarter, more connected care.
The Tools Changing the Game
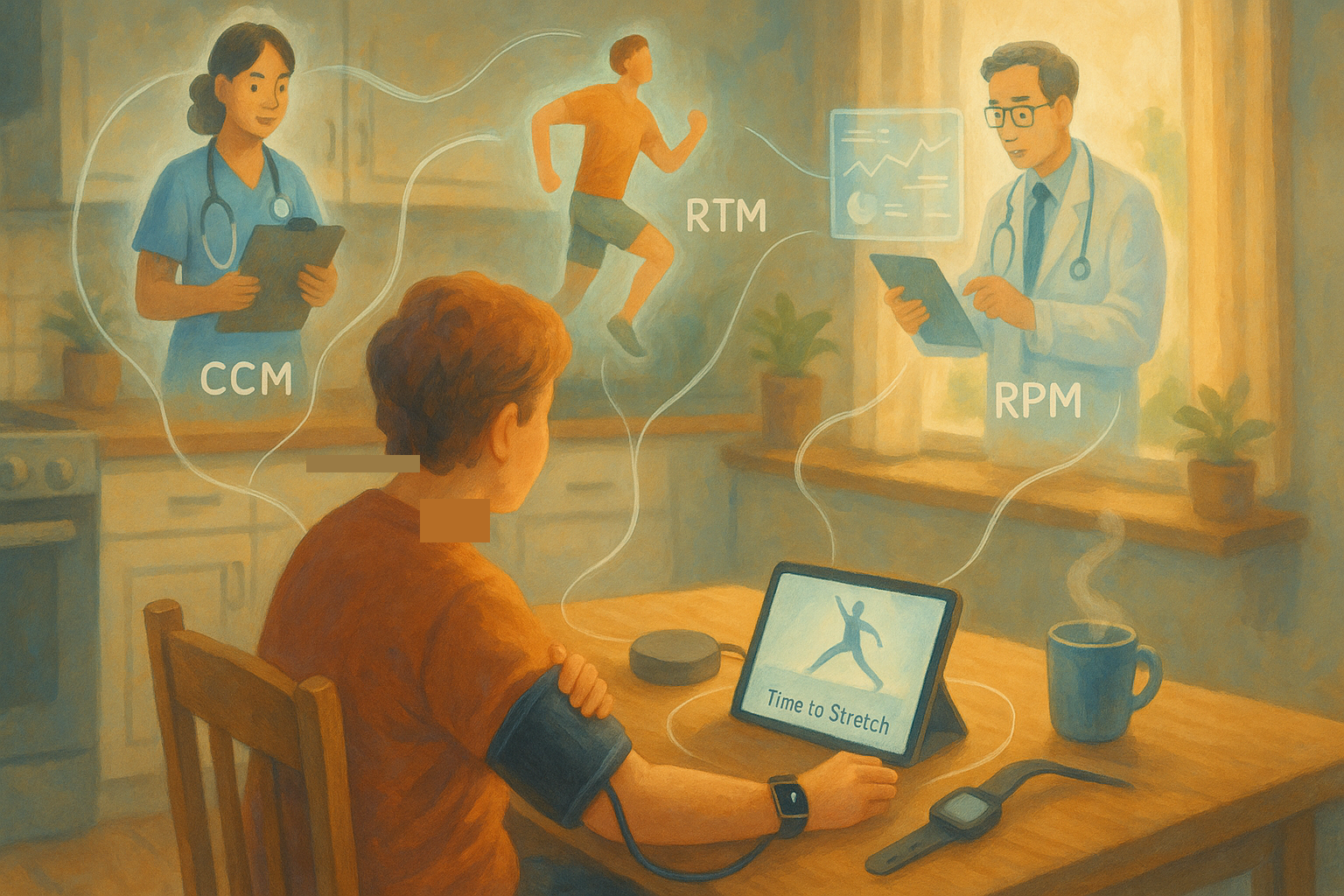
Let’s break down RPM, RTM, and CCM.
Remote Patient Monitoring (RPM) is a health guardian that’s always watching out for you. It uses at-home devices to track your heart rate, sleep, or blood pressure, sending that data straight to your doctor. For chronic pain, it’s an early warning system, if stress spikes your heart rate, your doctor can adjust your plan before pain takes over.
Remote Therapeutic Monitoring (RTM) is your treatment’s biggest fan. It tracks whether you’re doing your physical therapy, taking meds, or logging pain levels. A system might remind you to stretch or ask how bad your pain is today, giving your doctor real-time insights to tweak your care.
Chronic Care Management (CCM) is the glue holding your healthcare team together. For Medicare patients with multiple conditions, such as pain and diabetes, a coordinator checks in regularly, reviews your meds, and connects you with specialists. It’s care that sees the whole you.
These tools work best together: RPM gathers data, RTM focuses on pain-specific needs, and CCM keeps everything coordinated. They’re not just tech, they’re a lifeline.
A Story of Hope: Sarah’s Journey
Meet Sarah, a 42-year-old teacher from Ohio. After a car accident, chronic back pain turned her life upside down. She couldn’t stand long enough to teach, and constant doctor visits wore her out. Pain meds dulled the ache but left her foggy, and she felt like she was losing herself. Then her clinic introduced RPM, RTM, and CCM. Sarah got an at-home device to track her activity and heart rate, showing how stress worsened her pain. An RTM system guided her through physical therapy with daily reminders, while her CCM coordinator called weekly to manage her pain and hypertension, even connecting her with a counselor. Six months later, Sarah was back in the classroom, engaging her students with a smile. Her pain wasn’t gone, but it no longer controlled her. Stories such as hers show what’s possible, platforms such as Pain Scored say RPM can improve pain scores by over 2 points on a 10-point scale, a change that means everything.
Why These Tools Matter
The benefits of these tools are game-changing. For patients in rural areas or with mobility issues, they bring expert help without leaving home. By catching issues early, they cut down on ER visits and hospital stays, CMS says CCM saves millions by preventing complications. Real-time data means your care fits your life, not a generic protocol. RTM helps you follow through on therapy or meds, which is key for chronic pain. And CCM’s check-ins fight the loneliness pain can bring.
The evidence is clear. A 2023 study in Pain Medicine found RPM improved pain outcomes by 30% in fibromyalgia patients, and the CDC’s 2022 opioid guidelines push for non-drug options such as those RTM supports. These tools are grounded in science and human need.
Overcoming Challenges
Nothing’s perfect, and these tools have hiccups. Some patients, particularly those less familiar with technology, may find it challenging to use devices or systems consistently. Systems don’t always share data smoothly, and CMS billing rules are strict: RPM and RTM can’t be billed together, but both can work with CCM if you track time. Solutions? Pick user-friendly platforms such as FairPath by Intelligence Factory, train patients and staff, and stay on top of billing guidelines. It’s work, but the payoff, better care, is worth it.
The Future Is Bright
The world of chronic pain management is evolving fast. AI is starting to predict pain flares by analyzing RPM and RTM data, letting doctors act proactively. At-home devices might soon track stress hormones or posture, guiding therapy with precision. Telehealth could pair with these tools for virtual counseling, tackling pain’s emotional side. And with CMS expanding coverage for RTM and CCM, access is growing. Sharing these trends shows you’re not just keeping up, you’re leading the way.
Moving Forward Together
Chronic pain is tough, but RPM, RTM, and CCM are making it manageable. They’re not just tools, they’re hope for patients, efficiency for providers, and progress for healthcare. Share this post, comment with your experiences, or follow innovators in the field. If you’re a provider, explore these technologies. If you’re a patient, ask about them. Together, we can turn pain into possibility.