In-House Remote Care Programs Overview
What Are the Benefits and Challenges of Running RPM, CCM, and RTM Programs
In-House?
Healthcare organizations face a critical decision: should they manage Remote Patient Monitoring (RPM), Chronic Care Management (CCM), and Remote Therapeutic Monitoring (RTM) programs internally or outsource to external vendors?
What Are the Key Benefits of In-House RPM, CCM, and RTM Programs?
Operating RPM, CCM, and RTM programs internally provides healthcare organizations with full control over every aspect of patient care delivery. This autonomy enables complete customization of clinical protocols, care workflows, and patient interactions to align perfectly with organizational values and existing care standards.
Organizations can adapt programs in real-time based on patient feedback and clinical outcomes without waiting for vendor approval or lengthy implementation timelines. This flexibility allows for immediate responses to patient needs and regulatory changes.
How Does In-House Management Improve Care Continuity?
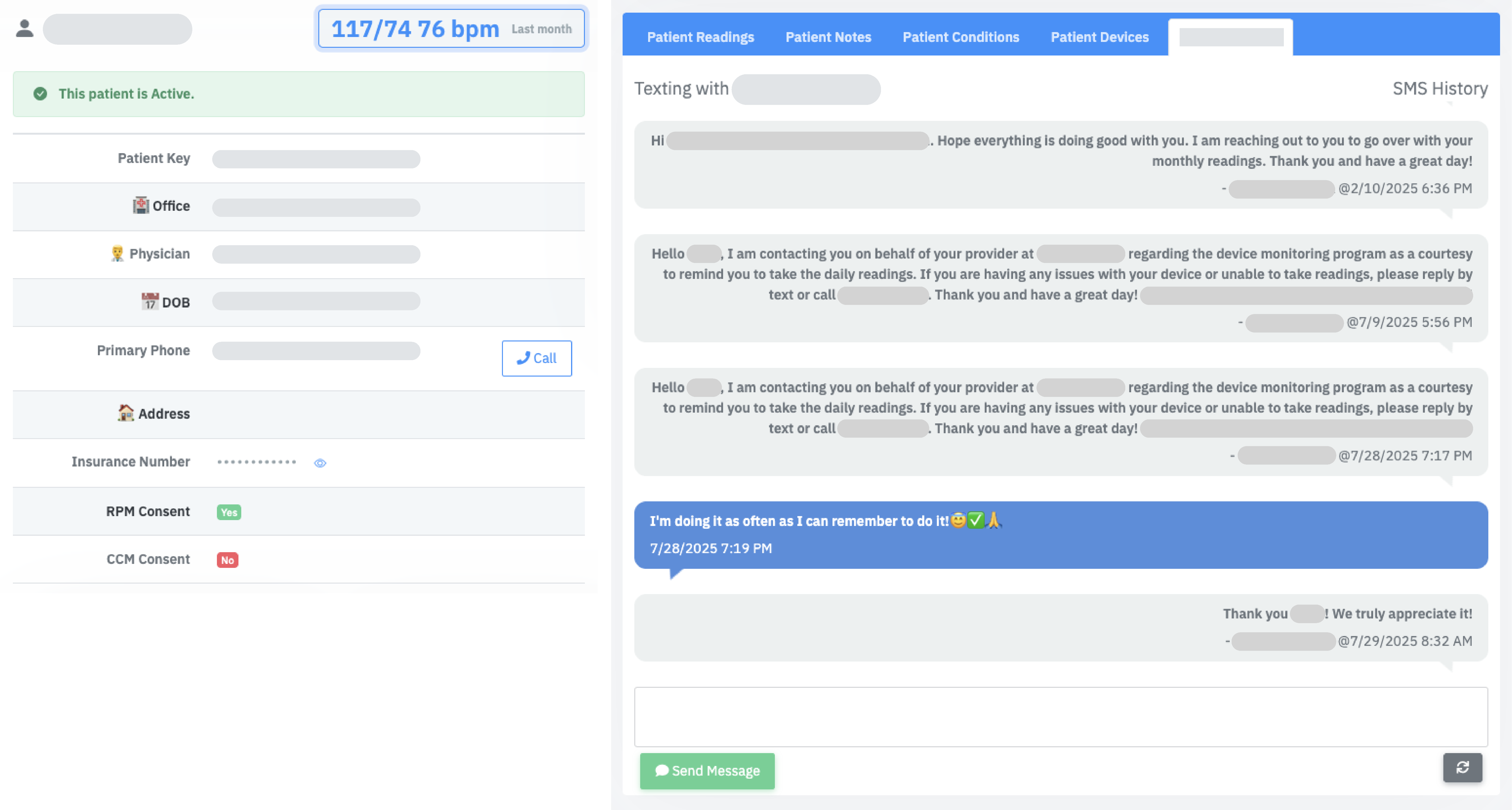
In-house programs create seamless integration with existing clinical workflows and electronic health record (EHR) systems. Patients benefit from consistent communication with familiar care team members who understand their complete medical history and personal preferences.
This continuity enables better coordination between primary care providers, specialists, and remote monitoring staff, resulting in improved patient satisfaction scores and superior clinical outcomes compared to fragmented vendor-managed programs.
What Are the Financial Advantages of Internal Program Management?
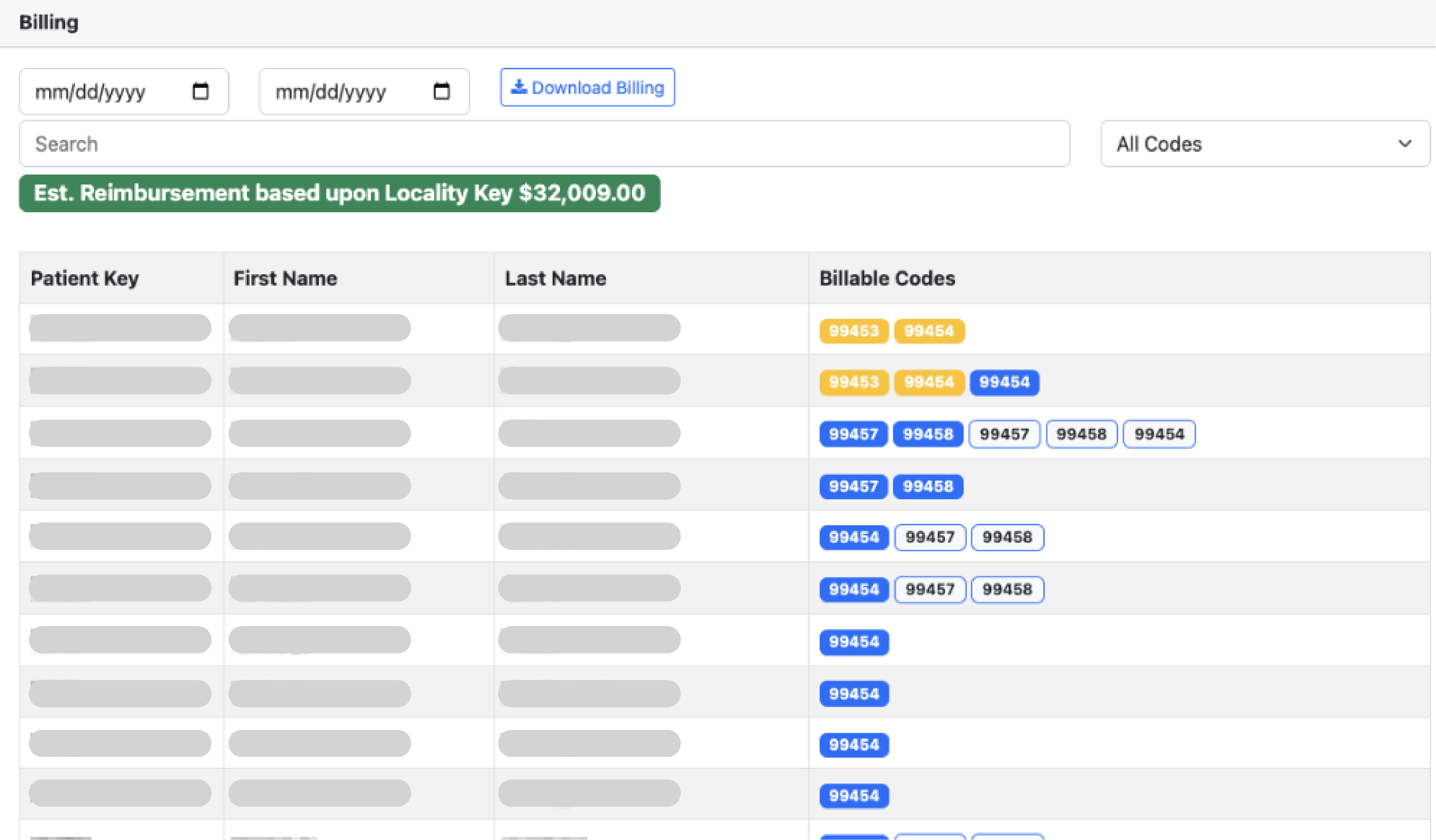
Direct billing and revenue management allows healthcare organizations to capture 100% of reimbursement potential from Medicare, Medicaid, and commercial payers. Without vendor fees or revenue-sharing arrangements, healthcare systems retain complete financial benefits while building sustainable long-term revenue streams.
Organizations maintain complete flexibility in pricing strategies and can quickly adapt to changing reimbursement landscapes, maximizing profitability from CMS billing codes including CPT 99453-99458 (RPM) and 99490-99491 (CCM).
How Does In-House Management Enhance Quality Control?
Internal program management provides direct oversight of clinical quality measures, staff training protocols, and regulatory compliance standards. Organizations ensure care delivery meets their specific quality standards and can implement improvements immediately based on performance metrics and patient outcomes.
This direct control proves particularly valuable for maintaining Joint Commission accreditation requirements, NCQA recognition standards, and Medicare quality reporting obligations without relying on third-party compliance.
Why Is Data Ownership Important for Healthcare Organizations?
All patient data, clinical outcomes, and program performance metrics remain within the organization's complete control, enabling comprehensive analytics and quality improvement initiatives. This data ownership supports internal research opportunities, population health management strategies, and evidence-based program enhancements.
Healthcare systems can leverage this data for value-based care contracts, risk adjustment modeling, and clinical research partnerships without sharing sensitive information with external vendors.
How Does In-House Management Address OIG Oversight Concerns?
The September 2024 OIG report
"Additional Oversight of Remote Patient Monitoring in Medicare Is Needed" highlighted significant oversight challenges with third-party RPM providers. The OIG found that about 43 percent of enrollees who received remote patient monitoring did not receive all 3 components of it, raising questions about whether the monitoring is being used as intended.
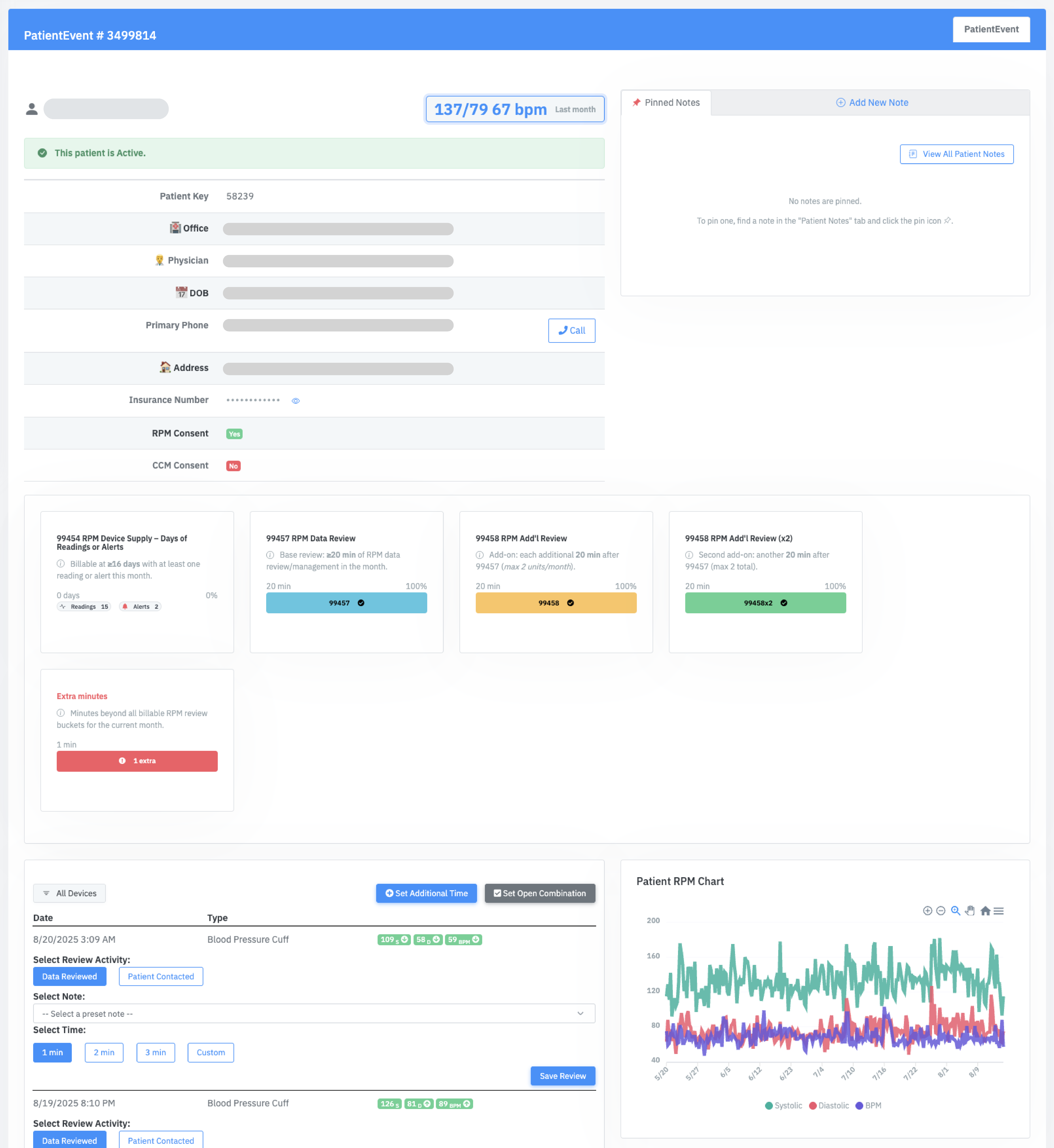
In-house programs provide direct control over all three RPM components: patient education and device setup (CPT 99453), device supply (CPT 99454), and treatment management (CPT 99457/99458). This ensures complete service delivery and reduces audit risk from incomplete care documentation that triggers OIG fraud investigations.
What Are the Main Challenges of Running Programs In-House?
What's the Investment Required for Remote Care Programs?
RPM, CCM, and RTM program implementation typically involves substantial upfront costs that vary significantly depending on program scope. These expenses cover program management software licenses, monitoring device inventory, clinical staff expansion, and ongoing operational requirements.
Beyond the initial setup, organizations also need to plan for continuous technology updates, staff training, and compliance systems—investments that can take over a year to generate returns. For many practices, especially smaller ones, this traditional approach creates budget constraints that can delay or prevent program launch altogether.
The FairPath Solution
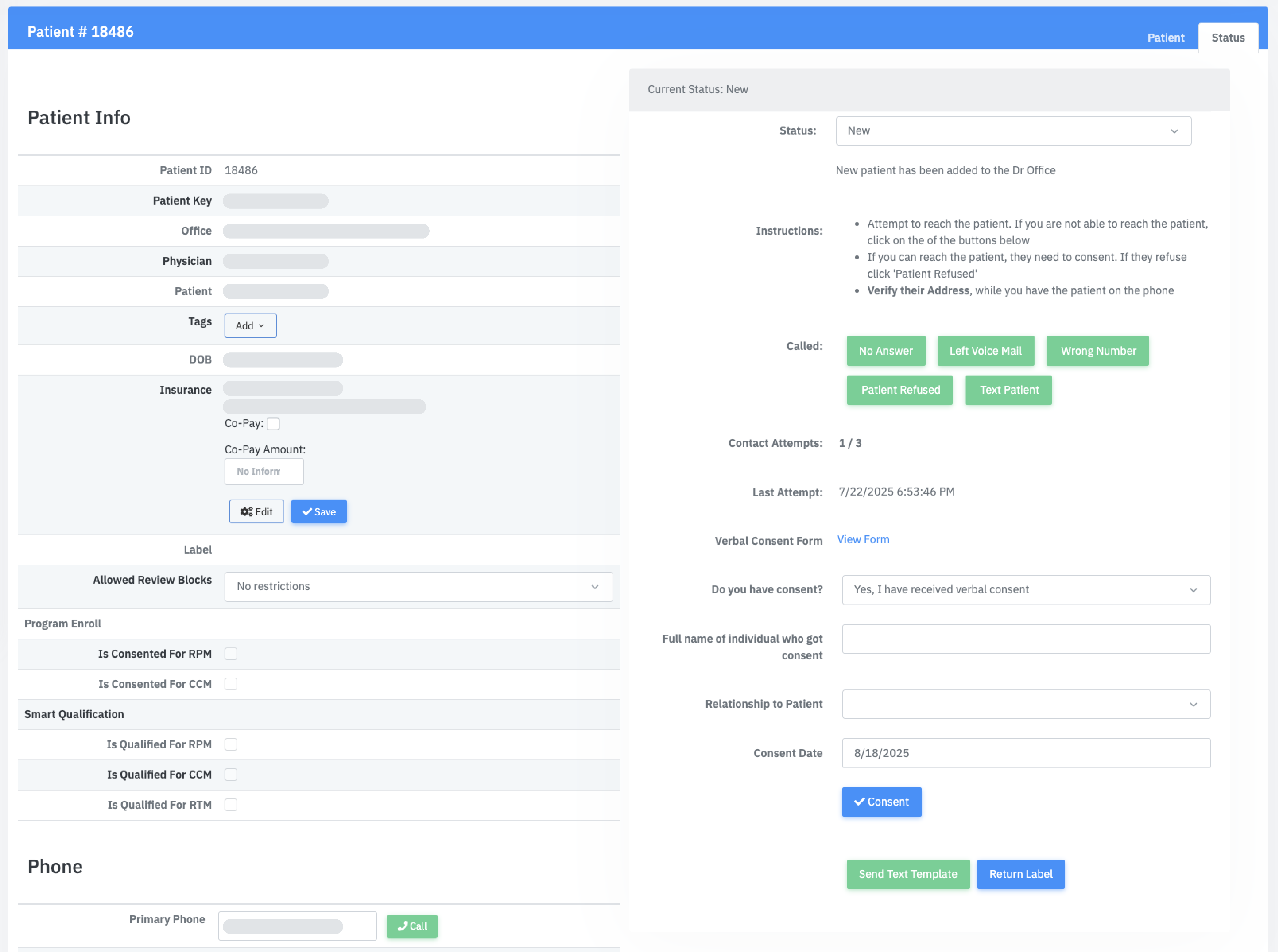
FairPath eliminates the need for large upfront investments. Through a simple flat fee per patient, you gain access to a comprehensive software suite that enables your practice to effectively run its own remote care program. FairPath was designed to help teams of all sizes—from small practices to large healthcare organizations—efficiently operate and scale these programs while delivering quality patient care and maintaining compliance and auditability.
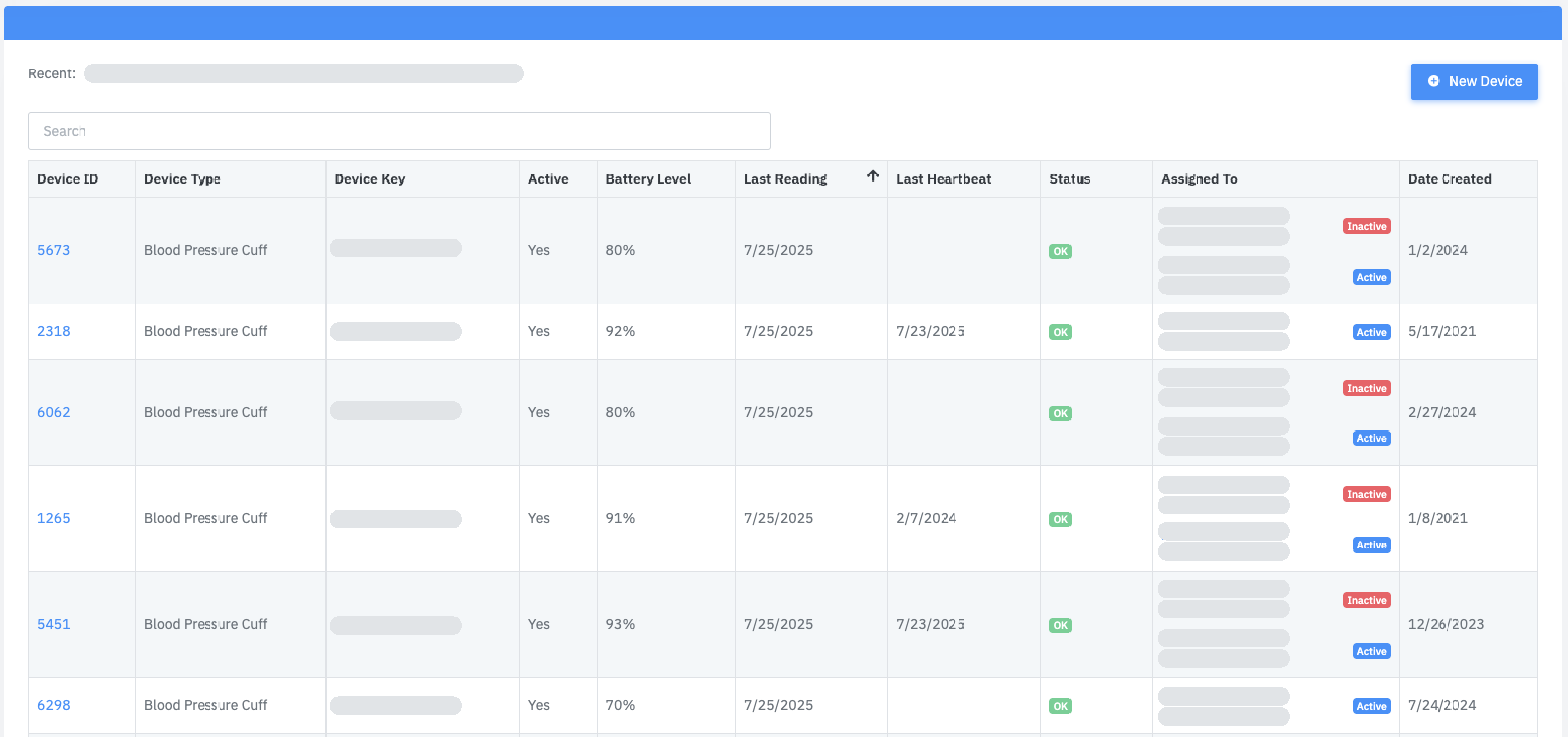
What Technology Infrastructure Challenges Should You Expect?
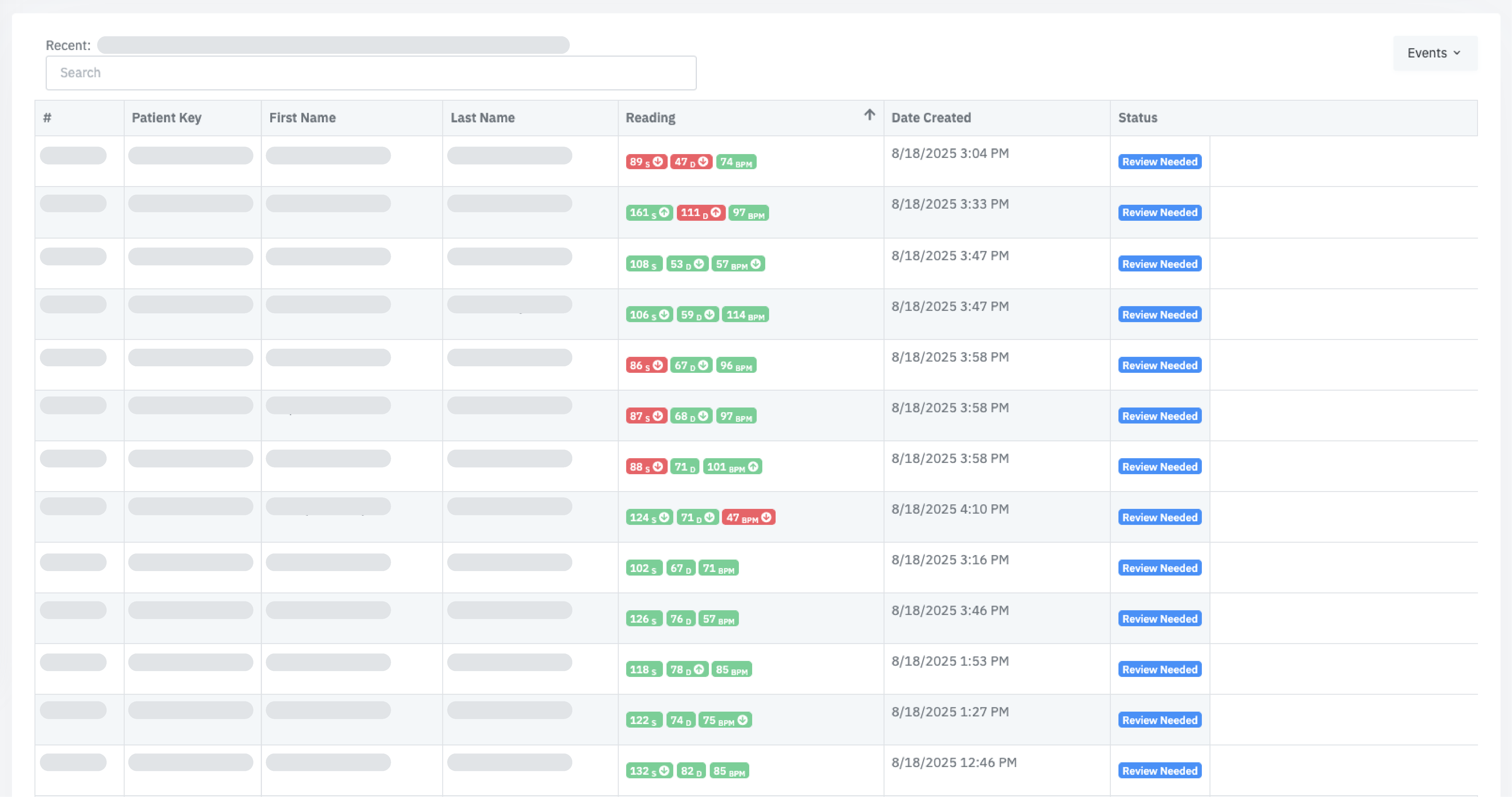
Successful programs demand robust technology platforms capable of seamless device integration, real-time data management, clinical workflow automation, and comprehensive regulatory reporting. Organizations must either develop these capabilities internally or invest in enterprise-grade software solutions.
Additional requirements include IT support for system maintenance, cybersecurity compliance for HIPAA regulations, data backup systems, and 24/7 technical support infrastructure that many healthcare organizations lack internally.
The FairPath Solution
FairPath was designed to address all these needs and has already been used to review millions of patient readings, generating revenue while preventing hospitalizations. The integrated AI technology provides complete audit trails and documentation for every patient interaction, code achievement, and clinical milestone. FairPath serves as the comprehensive technology infrastructure you need to successfully operate your own remote care program.
What Staffing and Training Requirements Are Involved?
RPM, CCM, and RTM programs require specialized clinical staff trained in remote care protocols, technology platform operation, and complex Medicare billing requirements. Organizations face challenges recruiting qualified registered nurses, care coordinators, and clinical supervisors in competitive healthcare employment markets.
Comprehensive training programs require 40-80 hours per staff member, covering clinical protocols, technology systems, billing compliance, and patient communication skills. Ongoing education requirements and staff turnover management add significant operational complexity.
The FairPath Solution
FairPath enables small teams to operate comprehensive remote care programs, and scale when needed. All clinical protocols and billing requirements are integrated into the AI-powered platform, and through Intelligence Factory's proprietary technology, updates to protocols, coding, and regulatory requirements can be implemented seamlessly. We also provide comprehensive training on program management, software utilization, and ongoing customer support.
How Complex Are Regulatory and Compliance Requirements?
Healthcare organizations must navigate intricate Medicare Advantage and traditional Medicare billing requirements, HIPAA privacy regulations, state telehealth laws, and CMS quality reporting obligations. The September 2024 OIG report identified significant compliance gaps, noting that Medicare lacks key information for oversight, including who ordered monitoring services for enrollees.
The OIG found that CMS cannot systematically identify companies providing RPM services because many RPM companies are not enrolled Medicare providers. This creates substantial audit risk for organizations using third-party vendors, as Medicare cannot track service delivery chains or verify appropriate clinical oversight.
In-house programs eliminate third-party compliance risks by maintaining direct control over ordering providers, service delivery documentation, and billing practices. Organizations can ensure proper physician orders, maintain complete claims documentation, and provide transparent audit trails that satisfy OIG recommendations for strengthened oversight.
The FairPath Solution
Intelligence Factory's proprietary technology enables FairPath to generate comprehensive, transparent audit trails that automatically adapt to regulatory changes in real-time. Whether responding to CPT code updates, the upcoming transition from ICD-10 to ICD-11, or evolving regulatory requirements, our system provides the tools and technology necessary to implement these changes seamlessly.
What Scalability Challenges Should You Anticipate?
As programs expand to serve additional patient populations and chronic conditions, organizations must proportionally scale technology infrastructure, clinical staffing, and operational processes. Managing growth while maintaining consistent quality standards and financial performance requires sophisticated resource planning.
Patient volume increases from 100 to 1,000+ enrolled patients demand corresponding increases in staff capacity, technology licensing, device inventory, and management oversight that can strain organizational resources.
The FairPath Solution
FairPath was designed for scalability: whether you're enrolling 100 or 1,000 patients, the system provides the tools and technology necessary to scale safely while maintaining compliance. FairPath's comprehensive onboarding and management module enables practices to track and manage every step of the program, including patient onboarding, consent documentation, device inventory management and integration, and device shipment coordination. The integrated proprietary technology also generates patient qualification scores for every patient, regardless of population demographics.