If you manage a Remote Physiological Monitoring (RPM) program, CPT code 99454 is likely your biggest source of revenue and, also likely, your biggest headache. This code, which reimburses for the supply of the device and data transmission, has long carried a notorious "all-or-nothing" requirement: the patient must transmit data on at least 16 separate days within a 30-day period.
If a patient transmits 15 days? You get $0. You lose money on the device, shipping, and cellular data, and Medicare pays you nothing.
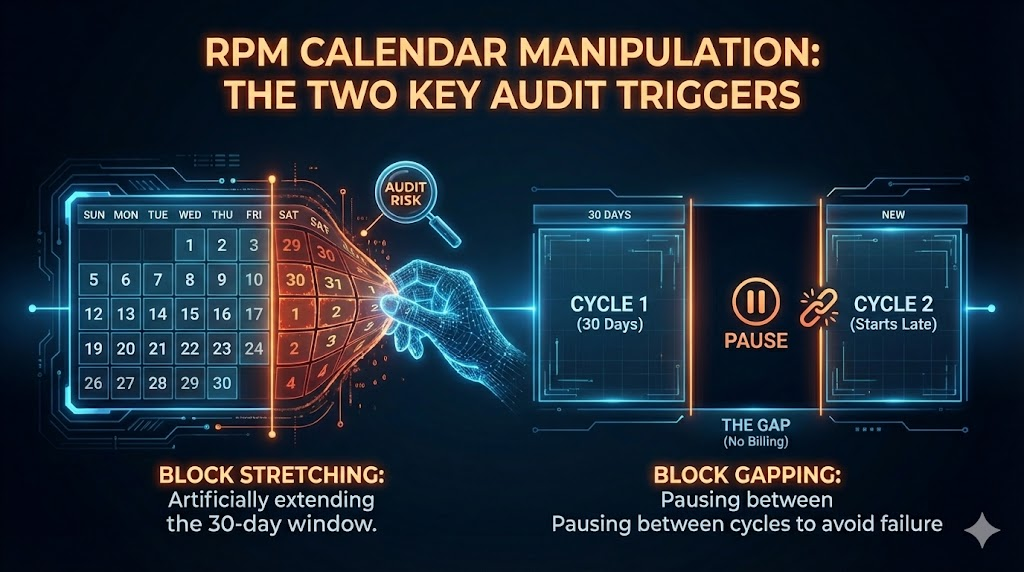
The financial pressure of this "reimbursement cliff" has driven some billing teams to devise creative (and dangerous) interpretations of the calendar to salvage lost revenue. Two strategies in particular have become popular, unfortunately:
Block Stretching and Block Gapping.
While they might sound like smart optimizations, they are compliance traps that can trigger federal audits. Here is exactly how they work, why they are dangerous, and the two valid ways to solve the problem.
The Illegal Trick #1: "Block Stretching"
The Mechanism:
Block Stretching is the attempt to lengthen the billing window to capture late data.
Imagine a patient is struggling with compliance. By Day 30 of their billing cycle, they have only transmitted 12 days of readings. You are four days short of the 16-day requirement. Instead of closing the month as a loss, you keep the "billing window" open. You wait until Day 45, by which point the patient has sent in 4 more readings. You now have 16 readings total. You bill CPT 99454 for this 45-day duration as a single unit of service.
Why It Seems Clever:
You aren't fabricating data. The patient did take 16 readings; they just took a little longer to do it. You argue that you are simply billing for a "unit of work" rather than a calendar month.
Why It Is Non-Compliant:
This violates the fundamental CPT descriptor for 99454, which explicitly states "each 30 days."
- The Violation: The code is time-based, not volume-based. The 30-day clock is a rigid, rolling window that begins the moment the device is set up. You cannot alter the unit of time (30 days) to accommodate the volume of data.
- The Trap: When you "stretch" Cycle 1 to 45 days, you are stealing 15 days from Cycle 2. This creates a "cascading delay" where your dates of service drift further and further away from the calendar year, creating impossible overlaps and gaps that are easily flagged by claims processing algorithms.
The Suspect Trick #2: "Block Gapping"
The Mechanism:
Block Gapping is more sophisticated. It involves stopping the clock between cycles to manipulate the start date of the next period.
Let's say a patient completes a successful 30-day cycle on January 30. You know this patient is erratic. If you start the next cycle immediately on January 31, they might fail. So, you program your software to "pause." You leave a 10-day gap (Jan 31 – Feb 9) where no billing cycle is active. You wait until you see the patient start transmitting data again on Feb 10, and then you start the clock for Cycle 2.
Why It Seems Clever:
You aren't stretching a single cycle; you are keeping your cycles strictly to 30 days (Feb 10 – Mar 11). You are simply choosing when to start them to maximize the probability of capturing 16 days. You argue: "Why should the clock tick if we aren't billing?"
Why It Is High-Risk (The "Free Device" Trap)
While technically distinct from stretching, Block Gapping invites scrutiny under two specific fraud statutes:
- The Anti-Kickback Statute (AKS): During that 10-day gap, the patient still has the expensive medical device in their home. If you aren't billing for it, you are essentially providing free equipment to a Medicare beneficiary. The OIG views free valuable technology as "remuneration" or an inducement to keep the patient in the practice.
- Medical Necessity (FCA): RPM is designed for chronic care management (e.g., heart failure, hypertension). These conditions do not take a 10-day vacation. By administratively pausing the service, you are creating a medical record that implies the patient didn't need monitoring for those 10 days. If they didn't need it then, why is it medically necessary the rest of the time? It creates a "Schrödinger's Patient", i.e.: sick enough to bill for, but healthy enough to ignore during the gaps.
If you are using a third-party RPM vendor and are unsure how these risks land contractually, it is worth pressure-testing the incentive model here.
The Two Valid Ways to Solve This
You don't need to manipulate the calendar to survive the 16-day rule. There are two compliant paths forward.
1. Use the New "Low-Volume" Codes (Starting Jan 1, 2026)
CMS has recognized that the 16-day rule is too harsh. Effective January 1, 2026, literally days from now, new CPT codes go live that solve this problem legally.
- The Fix: A new code, CPT 99445, pays for device supply when a patient transmits 2 to 15 days of data.
- The Strategy: Stop gapping and stretching. Maintain a strict, continuous 30-day calendar. If a patient hits 16 days, bill 99454. If they only hit 10 days, bill 99445. You get paid for the supply either way, without compliance risk.
2. Automate Utilization and Compliance with FairPath.ai
The root cause of "gapping" isn't usually malice; it's a lack of tools to drive patient behavior. FairPath.ai offers a dual solution that fixes the revenue problem at the source:
- Automated Billing Rules: FairPath's AI rigidly enforces compliant 30-day rolling windows. It prevents you from making illegal moves like "stretching" dates, ensuring every claim you submit allows you to sleep at night.
- Increasing Utilization: Instead of manipulating dates after a patient fails, FairPath helps your program succeed during the month.
- Intelligent Reminders: The system identifies patients at risk of missing the 16-day goal and sends targeted, AI-driven nudges to get them back on track.
- Gamification: By using engagement mechanics, FairPath encourages patients to build a habit of daily monitoring, naturally pushing them over the 16-day threshold.
- Clinician Tools: Better dashboards ensure your staff can intervene before a patient "drops through the cracks," securing your revenue without risking your license.
The Bottom Line: The 16-day rule is rigid, but with the 2026 codes just around the corner, the need for "clever" workarounds is over. Equip your practice with FairPath to handle the transition and turn compliance into a competitive advantage.
If you want to see how FairPath handles utilization, billing logic, and audit-grade documentation during this transition, you can explore it here.