If you are billing RPM for Diabetes, Hypertension, or COPD under UHC, your claims will likely be denied starting January 1st.
Related FairPath Resources
If UnitedHealthcare (UHC) is a significant payer for your practice, you need to audit your Remote Patient Monitoring (RPM) panel immediately.
Quietly buried in their December 2025 policy bulletins, UHC has announced a massive restriction on RPM coverage that goes into effect January 1, 2026 .
Unlike CMS, which is expanding remote care through new payment models like APCM, UHC is moving in the opposite direction. They are adopting a strict "proven vs. unproven" stance that effectively eliminates RPM coverage for the vast majority of chronic conditions.
The New HF/HDP Standard
Starting Jan 1, UHC will consider RPM "Proven and Medically Necessary" for only two primary indications:
- Heart Failure (HF)
- Hypertensive Disorders of Pregnancy (HDP)
For almost every other common chronic condition, including Type 2 Diabetes, Essential Hypertension, COPD, Anxiety, and Sleep Apnea , UHC has explicitly flagged RPM as "Unproven and Not Medically Necessary."
What This Means for Your Revenue
If you are currently billing codes 99453, 99454, or 99457 for a UHC patient with diabetes or standard hypertension, you face a high risk of automated denials beginning in the new year.
This applies across Commercial , Medicare Advantage , and Medicaid (Community Plan) lines of business.
Dont Panic. Pivot.
This policy change is aggressive, but it is manageable if you act before the deadline.
- You need to identify every UHC patient currently on RPM.
- You need to verify if they have a qualifying Heart Failure or Pregnancy diagnosis.
- If they don't, you need to transition them to Chronic Care Management (CCM) or other care models before Dec 31st to avoid revenue disruption.
Get the Red Alert Survival Guide
We have compiled a comprehensive resource breakdown of this policy update. It includes the specific policy numbers, a decision tree for your patient panel, and a guide on which "safe harbor" codes (like CCM and RTM) are still viable.
👉 Read the Full Guide: The 2026 UnitedHealthcare Remote Care Shift
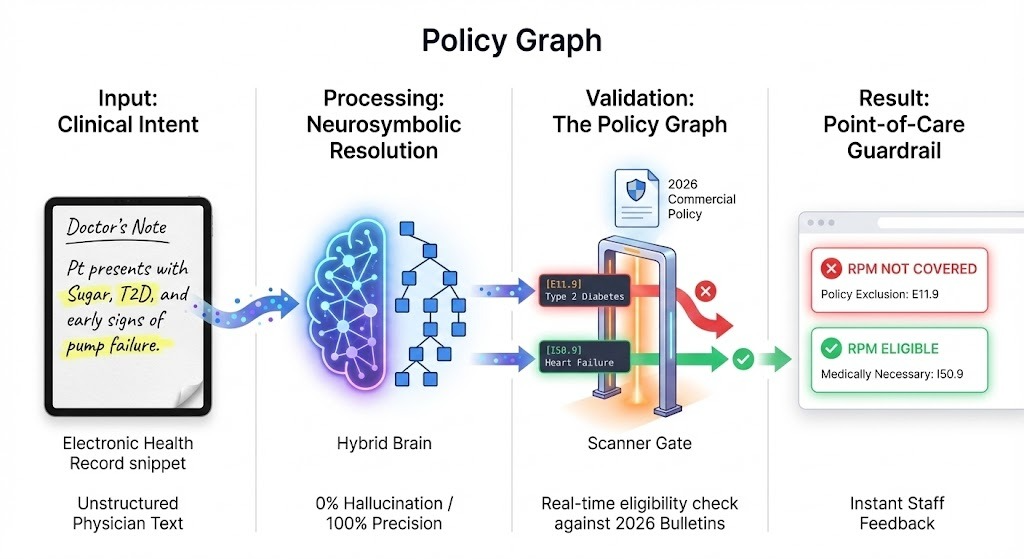
How We Automate This Rule
Reading the policy is one thing. Enforcing it across 2,000 patients is another. In FairPath, our Payer Ontology now reflects the 2026 UHC restrictions and automatically cross-references Payer (UHC) , Diagnosis (I10 vs I50.9) , and Program (RPM) so teams know where RPM is and is not covered.
- Patient records are evaluated against the updated UHC policy logic inside the Payer Ontology.
- When a UHC member is tied to a non-covered diagnosis for RPM, the enrollment workflow surfaces a clear “Not Covered” flag.
- Clinicians and staff can redirect patients into APCM/CCM-first pathways without wasting setup time or billing attempts.
Related Resources for Your 2026 Strategy
The UHC shift is just one part of a chaotic year for remote care. As you restructure your remote care program, use these tools to ensure you remain profitable and compliant:
- The CMS Strategy: While UHC restricts, CMS is expanding. Learn how to pivot to the new Advanced Primary Care Management model. Read the Guide: CMS 2025-26 APCM/RPM
- The Economics: Losing RPM coverage for UHC patients hurts. See how it impacts your bottom line if you are still paying a vendor. Run the Vendor Profit Analyzer
- The Compliance Check: With policies changing this fast, audits are inevitable. Ensure your documentation is bulletproof. Download the 2026 OIG Audit Survival Guide