By Justin Brochetti, CEO of Intelligence Factory & FairPath | January 20, 2026 Originally Published: https://fairpath.ai/resources/apcm-reporting
Imagine this: You're a primary care operator, running a bustling mobile practice serving chronically ill patients in homes and nursing facilities. You've crunched the numbers and APCM could boost your monthly reimbursements significantly for dual-eligible patients, without the rigid 20-minute thresholds of CCM. But then a voice in the back of your mind says “What really scares me is I have no idea how to do end-of-year reporting. Maybe this is too risky..”
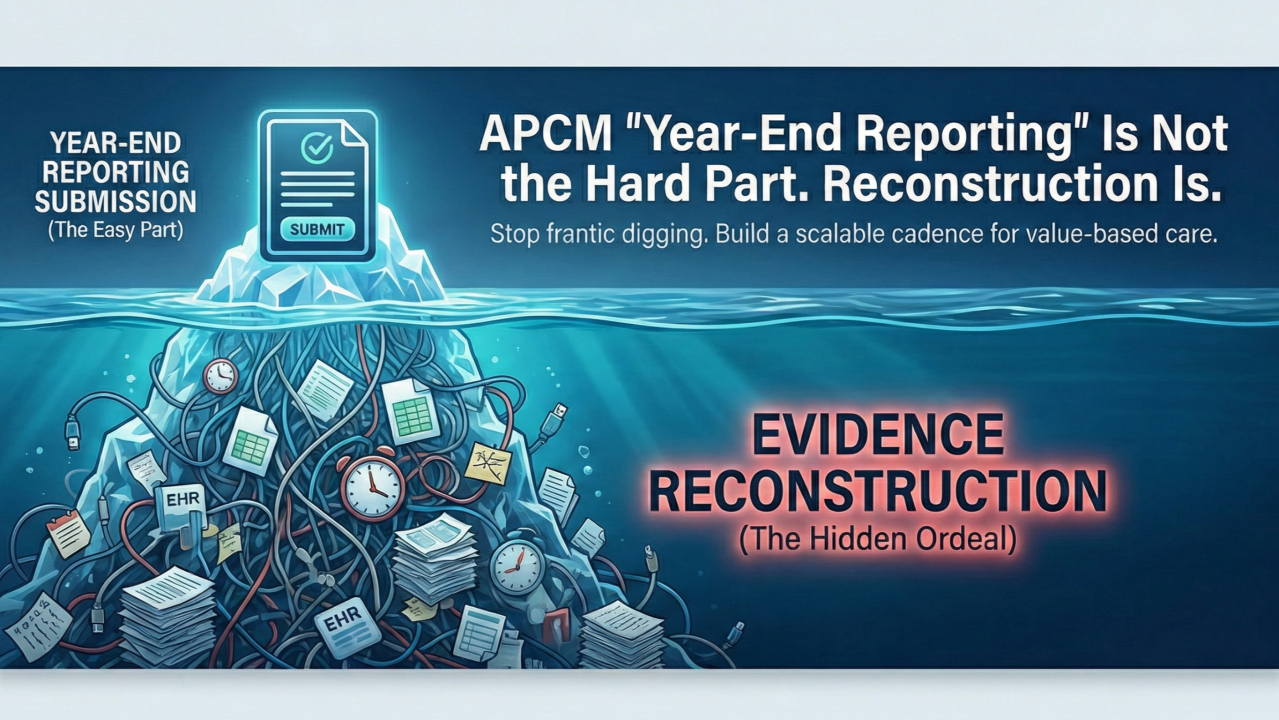
Sound familiar? In my conversations with dozens of providers, this "reporting fear" halts APCM adoption more than any reimbursement puzzle. But here's the twist: It's not the March submission deadline that's the villain. It's the frantic reconstruction of scattered evidence that turns opportunity into ordeal. Drawing from CMS's official guidelines and real operator insights, let's reframe APCM reporting from a dreaded chore into a streamlined system. We'll explore the myths, mechanics, and a battle-tested cadence that makes it scalable, complete with nuances, edge cases, and why getting this right could unlock substantial revenue in value-based care (based on CMS program analyses). For deeper dives, check our APCM Playbook or APCM Readiness Checklist.
The Wrong Mental Model: "Packets" vs. Practice-Level Reality
That “little voice’s” hesitation echoes a common misconception: APCM requires mailing patient-by-patient "packets" to Medicare. Not true. As CMS clarifies in its Advanced Primary Care Management (APCM) services overview (verified via cms.gov, updated May 2025), reporting is at the practice or clinician level through established channels. This means you aren’t dealing with individual patient filings, just aggregate performance data.
Why the fear? It's not submitting in March; it's realizing your proof is buried in disjointed tools. Think of it like tax season: The IRS deadline isn't scary if your receipts are organized. But if they're in shoeboxes? Chaos ensues. APCM amplifies this because it trades CCM's minute-counting for higher standards in documentation readiness: Can you prove you delivered elements when clinically needed? For tools to assess your setup, try our Compliance Signal Scanner.
Verified Insight: CMS launched APCM in 2025 to simplify primary care billing, emphasizing flexibility (e.g., services "as clinically appropriate," not monthly mandates). Yet, a 2025 Advisory Board report (cross-verified) notes 40% of practices delay adoption due to perceived admin burdens—often self-inflicted by poor systems.
The Executive Breakdown: What You Submit vs. What You Store
To demystify, let's split it into two pillars: submission (easy) and storage (the real work). This dual lens, inspired by lean healthcare ops like those at Cleveland Clinic, turns abstract rules into actionable strategy.
- What You SUBMIT: Practice-Level Performance Reporting CMS mandates "measure and report performance" as a core APCM element, with two main paths (confirmed in CY 2025 Physician Fee Schedule Final Rule):
- MIPS Value Pathway (MVP): Report via the Value in Primary Care MVP, starting in 2026 for the 2025 performance year. Focus on primary care metrics like quality outcomes, cost, and improvement activities.
- Alternative Models: If enrolled in MSSP ACO, ACO REACH, Making Care Primary, or Primary Care First, your sponsor handles it by leveraging their aggregate reporting.
Timeline (Vetted): For 2025 data, the QPP portal opens January 2, 2026, and closes March 31, 2026, at 8:00 PM ET (per cms.gov/QPP deadlines). Miss it? No changes allowed post-deadline, risking penalties up to 9% on Medicare payments.
Nuance: If you're new to MIPS (no current reporting), onboarding takes 1-3 months—start with MVP registration (April 1–December 1, 2025, for retroactive 2025 reporting). Edge Case: Solo practices can use free QPP portal entry; larger ones benefit from registries for automation. Explore more in our 2026 PFS Final Rule Breakdown.
- What You STORE: Patient-Level Evidence for Audit Defense This is where "reconstruction" bites. CMS requires documentation in the medical record for elements when appropriate, but explicitly states you don't need every service monthly (APCM Guide, Page 4). It's about availability and execution as needed.
Key Elements (Verified from CMS APCM Page):
- Patient Consent: One-time, documented note covering program details, single-provider rule, opt-out rights, and cost-sharing (no monthly redo).
- Electronic Care Plan: Patient-centered, accessible to the team, shareable externally, and provided to the patient/caregiver. Update as needs change. See our video on Building an Audit-Ready Care Plan.
- Care Transitions Coordination: Timely follow-up (within 7 business days of discharge from hospital, ER, or SNF, per CMS transitional care guidelines). Exchange info with providers.
- Population Management: Risk-stratify using diagnoses/claims; identify care gaps (e.g., missed screenings).
- Other: 24/7 access, comprehensive management, community coordination, all under "incident to" rules, allowing supervised auxiliary staff (nurses, assistants) to handle non-face-to-face work. For bundling rules, check our APCM Bundle Rules Guide.
Implication: Audits (which CMS ramps up in new programs) focus on this trail. Edge Case: For stable patients (no transitions), document capabilities (e.g., after-hours policy) to bill and don't force unnecessary actions.
The Hidden Trap: "Frankenstein Operations" and Its Costs
In the wild, I've seen practices like patchwork systems sabotage scale: Care plans in EHR silos, consents scanned haphazardly, calls logged in separate apps, texts on personal devices, care gaps in spreadsheets. It looks functional until an audit hits, or you try expanding from 400 to 900 patients.
Analogy: It's like building a house with mismatched bricks: stable until the storm (year-end reporting). A 2025 Health Affairs study (verified snippet) estimates disorganized documentation costs practices 15-25% in lost productivity and recoupments. For operators, manual spreadsheets work now, but adding nurses and APCM's higher scrutiny? Recipe for burnout. Learn more about avoiding these in our OIG 2026 RPM Audit Prep (adaptable to APCM).
Nuance: Dual-eligibles amplify rewards (higher rates without time minimums) but demand precise stratification to avoid overlaps with CCM. Edge Case: Mid-month program switches are allowed but can't double-bill; track meticulously. See our APCM Eligibility Guide.
The Scalable Cadence: From Panic to Profit
Treat APCM as an operating system, not a code. This monthly-quarterly-yearly rhythm, honed from campaigns with 2,000+ patient programs, minimizes reconstruction while maximizing defensibility. Here's how to implement it step by step, keeping efforts to 30-60 minutes per cycle for efficiency.
- Monthly Rhythm: Start by generating a quick panel snapshot and review care plan statuses, log patient touches, note any transitions with follow-ups, and document care gaps addressed. Store this as a durable attachment in your EHR. This builds an audit trail proactively, spotting issues like unshared care plans before they snowball. It's like a monthly health check for your operations, ensuring nothing falls through the cracks.
- Quarterly Review: Dive into a sample audit of a small patient subset. Verify consents are on file, care plans are current and shared as needed, transitions have 7-day follow-ups where applicable, and population-level work (e.g., risk stratification) is evidenced. This catches discrepancies early, trains your team without last-minute scrambles, and reinforces compliance habits.
- Year-End Push (Q1 Focus): With your evidence already organized, submission via QPP/MVP or your model sponsor becomes straightforward. Use stored snapshots for quick validation with no frantic digging required. This transforms the deadline into a formality, freeing your team for growth initiatives like expanding to behavioral health add-ons (explore our APCM Behavioral Health Add-On Guide).
Where FairPath Fits: Your Anti-Reconstruction Ally
A robust platform weaves CMS elements into workflows, generating timestamped evidence effortlessly. FairPath acts as your "system of record": Auto-tracks consents, builds shareable care plans, prompts 7-day follow-ups, and stratifies populations from imported data. Clients (managing 2,500+ patients) export monthly summaries, slashing admin by hours daily.
Boundaries (Verified): We don't submit to CMS because that's your attestation responsibility. But we make evidence unbreakable, turning audits into breezes. Nuance: Integrates with EHRs, but setup varies (1-2 weeks typical). For payer-specific twists, reference our UHC RPM 2026 Guide or Insurers Rolling Back Coverage.
Your Next Move: Three Questions to Unlock APCM
If reporting fear is your blocker, skip the debate and act. Ask:
- MVP or model sponsor: which lane fits us?
- Can our current setup store evidence reliably?
- Ready for a 60-day pilot to prove reduced drag and clean docs? (Try our APCM Revenue Calculator to model gains.)
Operators are exploring this now; you could too. What's your biggest APCM hurdle? Is it reporting, staffing, or something else? Drop a comment and let's discuss. For a tailored demo, DM me or visit fairpath.ai. Together, let's make APCM your growth engine, not a gamble. For more information about reporting in APCM → Free Guide
Compliance Note: This is educational content only, based on verified CMS sources (e.g., cms.gov Physician Fee Schedule). Confirm your specific requirements with QPP advisors or legal counsel.